In December 2025, India reported a fresh outbreak of the Nipah virus in West Bengal involving two healthcare workers and official confirmation and public health announcements were made in late January 2026. Authorities have since traced nearly 200 contacts, all of whom tested negative and declared the situation contained.
Yet the episode has reignited global concern over the Nipah virus. While rare and difficult to transmit, the virus carries a high fatality rate in those infected, which is why even small outbreaks receive close attention from health authorities.
What is the Nipah Virus?
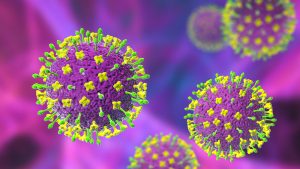
Source: Shutterstock (1) and (2)
The Nipah virus (NiV) was first identified in Malaysia in 1999. It belongs to the Paramyxoviridae family and is closely related to the Hendra virus. Fruit bats of the Pteropus genus are their natural reservoir.
WHAT IS A NATURAL RESERVOIR?
An animal species that naturally carries a pathogen and can transmit it to humans, often without showing signs of illness.
The Nipah virus has a high fatality rate (40–75%). It can spread directly from person to person and has no approved vaccine or treatment, making it a health concern.
Each outbreak raises fears of wider spread because of its ability to cause severe neurological disease, respiratory illness and long-term complications in survivors.
The World Health Organization (WHO) has identified Nipah virus as one of the top emerging pathogens with pandemic potential, listing it as a priority disease for research and preparedness.
Origins in Malaysia and Singapore
The Nipah virus was first identified in Malaysia around 1998 to 1999, when pig farmers began suffering from severe encephalitis.
265 cases were confirmed, with 105 deaths, a fatality rate of around 40%. The outbreak spread to Singapore, where abattoir workers handling imported pigs were infected, resulting in 11 cases and one death.
The virus spread from fruit bats (Pteropus species) to pigs, then to humans. To halt transmission, Malaysia culled over one million pigs, devastating its pig farming industry. Since then, the virus has not been reported in either country.
Spread to India and Bangladesh
Since its discovery in Malaysia in 1999, the Nipah virus has spread to India and Bangladesh, with Bangladesh experiencing repeated outbreaks almost every year since 2001. These outbreaks have made Nipah one of the most closely watched zoonotic diseases in South Asia.
In 2001, the first Nipah outbreak outside Malaysia happened in West Bengal, with dozens of cases and high fatality. Between 2018 and 2023, multiple outbreaks were recorded in Kerala. Each case was contained, yet still resulted in significant mortality.
India’s outbreaks often involve direct bat-to-human transmission or human-to-human spread in hospitals.
The first outbreak in Bangladesh happened in 2001. It was linked to the consumption of raw date palm sap contaminated by fruit bats.
Following that, Bangladesh has reported almost annual Nipah flare-ups since then, with case fatality rates often exceeding 70%. The virus’s spread was often caused by drinking raw date palm sap and being in close contact with infected patients.
WHAT DOES “CLOSE CONTACT” MEAN?
It refers to being within arm’s reach of an infected person for prolonged periods, like sharing utensils, caring for them without protective gear, or exposure to their saliva, respiratory droplets, or bodily fluids.
Bangladesh experiences repeated outbreaks of Nipah because:
- Fruit bats (Pteropus) are common across rural Bangladesh.
- Collection and consumption of raw date palm sap provides a direct route for bat-to-human transmission.
- Limited infection control in rural hospitals has allowed human-to-human spread.
- Dense populations and close human–animal interactions increase risk.
How the Current Situation Differs
In terms of scale, the Malaysian outbreak involved hundreds of cases and required mass pig culling. In contrast, the current Indian outbreak has so far affected two healthcare workers.
Also, Malaysia’s outbreak was linked to pigs, which served as amplifying hosts. In India, transmission is believed to be direct from bats or human-to-human, with no pig involvement.
During the outbreak, Malaysia faced widespread agricultural and economic disruption. In contrast, India’s outbreak was quickly contained through contact tracing and hospital infection control measures.
Both outbreaks triggered international concern, but India’s rapid containment highlights improved surveillance and preparedness compared to the late 1990s.
Should the Public Be Worried?
Since the Nipah virus does not spread through the air, the current outbreak has been small and contained, with no evidence of wider community spread. Furthermore, modern surveillance, rapid testing and strict hospital protocols have helped prevent escalation.
Despite that, Nipah’s high fatality rate, ability to spread between humans and lack of treatment or vaccine mean that even a few cases demand serious attention. The virus’s reservoir in bats also makes sporadic outbreaks likely in South and Southeast Asia.
That said, while the public need not panic, experts stress the importance of awareness, hygiene and vigilance to prevent future flare-ups.
How does the Nipah Virus Spread?
- Through direct contact with infected animals (especially bats or pigs).
- Consuming contaminated food, such as raw date palm sap tainted by bat saliva or urine.
- Via close contact with infected people, particularly in healthcare settings.
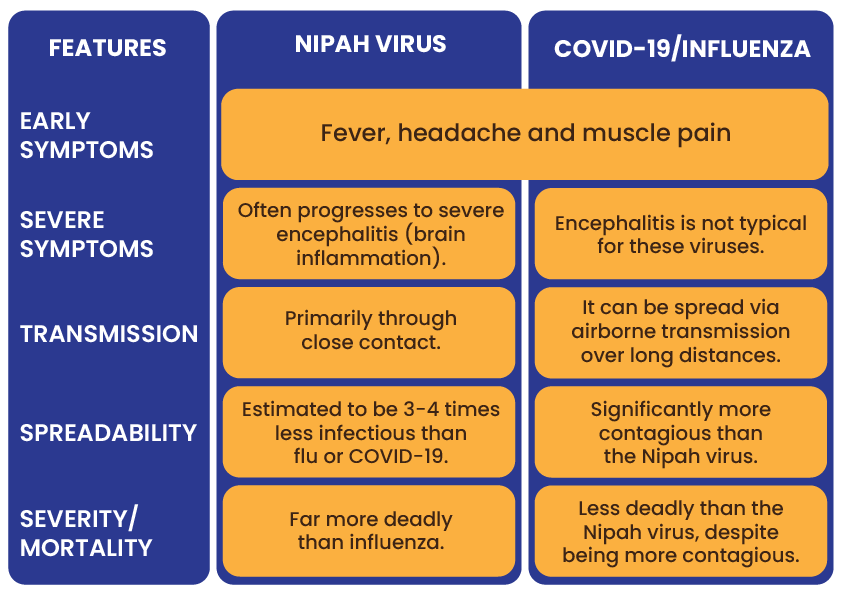
Is Nipah Similar to COVID-19 or Influenza?
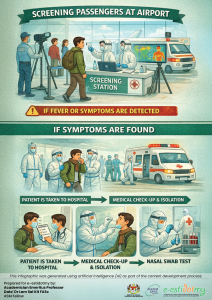
What Precautions are Countries Taking at Airports?
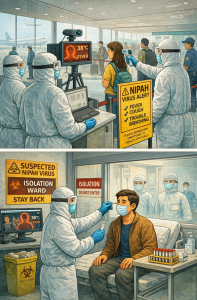
- Thermal screening: Passengers are scanned for fever using thermal cameras as well as for flu-like symptoms such as cough, breathing difficulty or confusion.
- Health declarations: Travelers complete questionnaires/forms detailing recent travel history, exposure risks and symptoms.
- Isolation protocols: Anyone who shows signs of illness is immediately separated and referred for medical evaluation.
- Testing if necessary: Suspected cases may need to undergo rapid diagnostic tests or be quarantined until results are confirmed.
What Simple Preventive Steps Can Individuals Take?
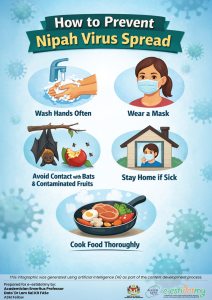
- Wash your hands frequently with soap and water.
- Avoid consuming raw drinks and fruits that bats may have contaminated.
- Wear a mask in crowded places and follow the Ministry of Health’s instructions.
- Seek medical care promptly if fever, headache, or neurological symptoms develop after possible exposure.
Conclusion
Since the first two cases were detected in December 2025, no new Nipah infections have been reported for over a month, making wider spread unlikely.
Nipah spreads only through close contact, and new cases would have appeared by now if community transmission were occurring.
While Nipah is less contagious than COVID-19 or the flu, it is dangerous due to its high fatality rate and lack of treatment. There is no cause for panic, but continued vigilance and good public health practices remain important.
Nipah is a reminder of the need for preparedness, but not a reason for fear.
Prepared by:
Academician Professor Emeritus Dato’ Dr Lam Sai Kit FASc
Senior Fellow